En-do-me-tri-o-sis is present in one third of women who suffer from infertility and in more than eighty per cent of women who suffer from chronic pelvic pain. It is a disorder that affects women in their 20s and 30s. Most women who have endometriosis do not have pain or infertility. Pain due to endometriosis typically starts a few days before the period only to become excruciating during menses. Some women complain of constant pain throughout the month. Also, endometriosis can become imbedded in the bladder and bowel causing bleeding with urination and bleeding with bowel movements.
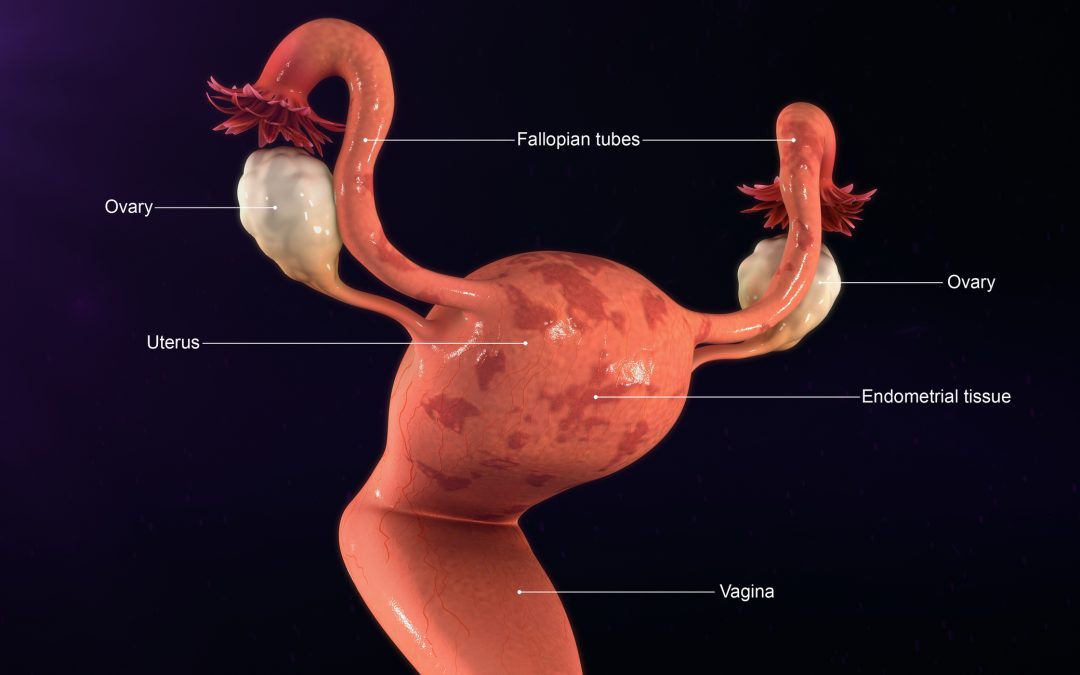
The simplest description of this disorder: tissue that lines the inside of the uterus attach to the outside of the uterus and ovaries. The most commonly accepted theory of how this happens is, when we have a period, although most of the blood and tissue comes out of the vagina, some of it backs up into the fallopian tubes, spilling onto the outside of the uterus and onto the ovaries. This process happens in all women and the body’s immune system usually clears away the blood and tissue. For reasons that are not quite clear, instead of being cleared, the tissue implants on the surface of the uterus, the ovary, the bowel or bladder and the surfaces between these organs. Implants that are deep or that are close to nerve ending cause more pain. I’ve done laparoscopic surgeries on women where the pelvis looks as if someone poured dark honey inside.
Women who start having periods before age eleven, whose periods come more often than every 27 days and who have heavy periods are more likely to develop endometriosis. Those who have family members with this disorder, i.e. sister or mother, also have a tendency to develop endometriosis. Having children, breast feeding and exercising may be “protective”.
The only way to definitely diagnose endometriosis is to biopsy the implant. A biopsy is important because implants can be varied in appearance and not always obvious to the surgeon. Undergoing surgery, whether laparoscopic (using a small camera to look inside) or by making a larger incision, means accepting the risk of bleeding, infection, injury to the bowel, injury to the bladder as well as the potential complications of general anesthesia. Ultrasounds, Cat Scans and MRIs cannot detect endometriosis. These tests can only reveal if an endometrioma (a cyst filled with endometriosis) has formed.
In women who have symptoms that suggest endometriosis, starting medical treatment without surgery may be the best way to proceed. The first line of treatment is a birth control pill, along with anti-inflammatory drugs like Naproxen or Ibuprofen. If the birth control pill fails to control pain, there are three other FDA approved drugs (androgens, GnRH agonists, progestins) that have been shown to be very effective in the treatment of endometriosis. All of these medications, including the pill, work by suppressing the amount of estrogen being produced by the body; this “cools” the implants, helping them to degenerate and thereby reducing pain. Medications used to treat endometriosis can have unpleasant side effects, like hot flashes and unwanted hair growth. Hormones are prescribed to treat bothersome side effects. Some of these medications, the GnRH agonist for example, can only be used for up to one year. Unfortunately, pain usually returns after women are off treatment. Birth control pills, however, can be used for years, is the least expensive and has the least side effects of all the medicines used to treat endometriosis. If they work don’t stop taking them, even if you’re feeling better!
Surgery to laser or burn the implants is effective but, again, after a few months most women report the return of pain. In those whom the implants have damaged the fallopian tubes or for women who are infertile because of endometriosis, Invitro fertilization (IVF) is the best way around this problem. Surgery is definitely needed if one has an endometrioma. Endometriomas can get very big, can cause the ovary to twist and cut off its blood supply and can rupture (pop open) in the pelvis. Removing them will reduce pain and in some cases, help with infertility.
Of course, there is always the option of a hysterectomy to remove the uterus and ovaries. One study showed that women whose ovaries were removed were least likely to have a recurrence of pain. But, another study showed that if the ovaries were free of implants and otherwise normal, leaving the ovaries in place was also an alternative. Removing the ovaries means instant menopause! Each woman has to weigh the benefits of ridding herself of pain verses living with hot flashes, vaginal dryness and other changes that come with menopause. Keep in mind that there are treatments for the symptoms of menopause but nothing will equal the benefits of hormones from the ovaries.
There you have it! Now spread the word!